- Eleonora Greco
- Original Article
Diagnostic and therapeutic impact of clinical bed-side ultrasonography in management of critically ill patients in High Dependency Unit
- 2/2017-Giugno
- ISSN 2532-1285
- https://doi.org/10.23832/ITJEM.2017.004
Eleonora Greco1, Emanuele Pivetta2, Maria Teresa Spina3, Marina Civita4, Gian Alfonso Cibinel4
- Emergency Department ASL 19 AT, Cardinal Massaia Hospital, Asti (AT), Italy
- Città della Salute e della Scienza di Torino University Hospital, Turin (TO), Italy
- Emergency Department, ASST Lodi, Italy
- Emergency Department ASL TO3, E. Agnelli Hospital, Pinerolo (TO), Italy
Abstract
Introduction
Methods
Results
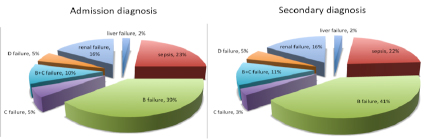
Figure 1: pathophysiological mechanisms of diseases identified as ‘admission’ and ‘secondary’ diagnosis
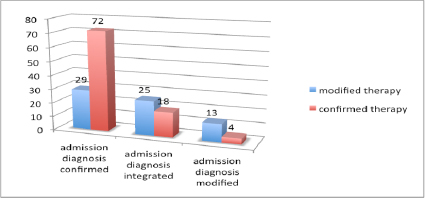
Figure 2: Confirmed/integrated/modified ‘admission’ diagnosis
Discussion and Conclusions
Based on our results, the ‘whole body’ US protocol, as integration of physical exam of the patient admitted in an HDU, might be considered useful for improving diagnostic accuracy and therapeutic management of critically ill patients.
Our US protocol suggested a significant impact on the ‘admission‘ diagnosis. It was ‘integrated’ in 27% of cases and ‘modified’ in 10% of cases. Furthermore the US protocol improved the identification of the pathophysiological and causal mechanisms underlying clinical syndromes and organ failures presented at admission in the HDU. This was true in particular for patients diagnosed with B failure where US evaluation was useful for redirecting the causal diagnosis towards a cardiogenic and/or a pulmonary syndrome.
In patients diagnosed with sepsis, our US protocol was useful for the identification of the septic source and this was useful in order to target the anthibiothic empirical therapy[5].
In conclusion a ‘whole body’ US protocol for evaluation of patients admitted to the HDU from the ED or other units might improve the clinical management allowing to better define the pathophysiological and causal mechanisms underlying presentation syndromes.
Aknowledgments
References
- A. E. Jones, V. S. Tayal, D. M. Sullivan, J. A. Kline: Randomized, controlled trial of immediate versus delayed goal – directed ultrasound to identify the cause of nontraumatic hypotension in emergency department patients. Crit Care Med 2004 Vol. 32, No 8
- SA Haydar, ET Moore, GL Higgins, CB Irish, WB Owens, TD Strout. Effect of bedside ultrasonography on the certainty of physician clinical decisionmaking for septic patients in the emergency department. Ann Emerg Med. 2012 Sep; 60 (3): 346 – 58.
- DA Lichtenstein. Point-of-care ultrasound: Infection control in the intensive care unit. Crit Care Med. 2007 May; 35 (5 Suppl): S262 – 7
- E. Manno, M. Navarra, L. Faccio, M. Montevallian, L. Bertolaccini, A. Mfochivè, M. Pesce, A. Evangelista. Deep Impact of Ultrasound in the Intensive Care Unit: The ICU – Sound Protocol. Anesthesiology, V 117, No 4, October 2012
- A. Leligdowicz, P. M. Dodek, M. Norena, H. Wong, A. Kumar, A. Kumar: Association between Source of Infection and Hospital Mortality in Patients Who Have Septic Shock. American Journal of Respiratory and Critical Care medicine Vol. 189, No 10, May 2014.

