- Lucio Brugioni
- Original Article
The non-invasive mechanical ventilation: the experience of the department of Internal Medicine and Critical Area of the Polyclinic Hospital of Modena
- 2/2017-Giugno
- ISSN 2532-1285
- https://doi.org/10.23832/ITJEM.2017.013
Brugioni Lucio, Benatti Piero, Mazzali Eleonora, de Niederhausern Francesca
Department of Internal Medicine and Critical Area
University Polyclinic Hospital of Modena
Abstract
Acute respiratory failure (ARF) is a deficiency of the respiratory system that causes an alteration of normal levels of oxygen and/or carbon dioxide in the blood.
ARF may be due to alterations in gaseous diffusion in alveolar-capillary level (type “1” acute respiratory failure), or to alterations in the functioning of the respiratory pump (type “2” acute respiratory failure) or to an association of the above causes.
ARF specific etiological treatment must be associated to oxygen administration, through ventilation, which may be spontaneous or mechanical (non-invasive or invasive).
The actual study describes experience about non-invasive mechanical ventilation in the department of Internal Medicine and Critical Area of the Polyclinic Hospital of Modena, from 2010 to 2014, examining clinical parameters and outcomes.
ARF may be due to alterations in gaseous diffusion in alveolar-capillary level (type “1” acute respiratory failure), or to alterations in the functioning of the respiratory pump (type “2” acute respiratory failure) or to an association of the above causes.
ARF specific etiological treatment must be associated to oxygen administration, through ventilation, which may be spontaneous or mechanical (non-invasive or invasive).
The actual study describes experience about non-invasive mechanical ventilation in the department of Internal Medicine and Critical Area of the Polyclinic Hospital of Modena, from 2010 to 2014, examining clinical parameters and outcomes.
Respiratory failure is a condition in which the respiratory system is not able to adequately carry out its gas exchange functions, such as oxygenation of the arterial blood and/or elimination of carbon dioxide from the venous blood.
Conventionally, (1),(2),(3) respiratory failure is defined in case of:
- Partial pressure of arterial oxygen (PaO2) <60 mmHg;
- Partial pressure of carbon dioxide in the arterial blood (PCO2)> 45 mmHg;
- Association of both previous.
You can distinguish two types of acute respiratory failure(4)(ARF):
- ARF type “1”, with gas exchange impairment and hypoxemia (associated with hypo/normocapnia). The pathophysiological mechanism behind is an important intrapulmonary shunt with changes in ventilation/perfusion ratio.
Generally diseases responsible for this condition are acute pulmonary edema, ARDS, severe pneumonia and pulmonary embolism. - ARF type “2”, with hypoventilation and hypercapnia.
It is caused by a reduction of the ventilation volume/minute or by an increase of physiologic dead space. Among the most common diseases there are neuromuscular diseases, myopathies, chronic obstructive pulmonary disease (COPD), bronchial asthma and restrictive lung disease.
The two types of respiratory failure are closely connected and can evolve into one another.
The ARF therapy can be divided into:
- Etiological therapy: it is directed to the treatment of the specific cause that induced ARF, it can be delivered with inotropic agents, antibiotics, bronchodilators, steroids etc.
- Supportive therapy (or symptomatic): aimed at correcting hypoxemia and respiratory acidosis, is indicated in all respiratory insufficiencies and it is based on the administration of O2 and postural therapy.
Ventilation can be spontaneous (delivered by low or high flow systems) or mechanical.
Mechanical ventilation is classifiable under invasive ventilation (IMV) or non-invasive (NIV).
The IMV provides the invasion of the patient’s airways to put them in communication with the respiratory system. It can be through tracheal intubation or tracheotomy and it’s a relevant method adopted by resuscitation intensive departments and partly by respiratory diseases departments. The NIV despite is a method that requires training and experience to be used optimally, it has the advantage to be used in emergency medicine departments and in other departments from specialists who are not resuscitators or pulmonologists. Moreover, compared to the IMV, the NIV offers the following advantages: reduction in the respiratory work, absence of complications related to prosthesis, possibility of avoiding sedation required for the IMV, conservation of laryngeal functions and cost reduction.(5)
The NIV techniques most used in emergency medicine departments are CPAP (Continuous positive airway pressure) and BiPAP (or BiLevel – BiLevel positive airway pressure) CPAP provides a predetermined positive pressure, greater than atmospheric, which is maintained constant throughout the respiratory cycle, and it improves oxygenation by increasing the functional residual capacity, favouring the recruitment and the patency of the alveoli excluded from the ventilation and improving the relationship between ventilation and perfusion.
The main indications for CPAP are acute cardiogenic pulmonary edema (ACPE), hypoxic and not hypercapnic ARF, obstructive sleep apnea syndrome (OSAS); atelectasis. (8),(9),(10)
BiPAP provides two different levels of positive pressure, which are an inspiratory positive airway pressure (IPAP) and an expiratory positive airway pressure (EPAP).
BiPAP facilitates the removal of air exhaled and prevents cases of re-breathing of CO2. It also reduces the patient’s work of breathing. The main indications to BiPAP are hypercapnic ARF, chronic obstructive pulmonary disease (COPD) exacerbation, pneumonia, neuromuscular disorders, dysfunction of the respiratory center (sedation/intoxication), shock (cardiovascular/septic). (11), (12)
Premises to the study
The NIV technique has spread in the last years also in semi-intensive care areas of Emergency Medicine and in Internal Medicine departments, and it continues to be adopted by the departments of Intensive Care and Pulmonary Intensive Care.
In January 2009, the department of Respiratory Diseases of the Polyclinic Hospital of Modena underwent a transfer of seat, resulting in temporary reduction of beds. This resulted in the need to find other places where treating patients with ARF requiring NIV. The close collaboration with the Respiratory Diseases department allowed the medical and nursing staff of the Internal Medicine and Critical Area department (IMCA) to undertake a training course to learn the methods of use of such therapy. Therefore, from May 2010, the IMCA department could cure patients suffering from ARF by treating them with NIV by two fans (Knight Star 335 – Puritan Bennett®), both in CPAP and BiPAP mode.
In the department a mode of NIV in CPAP ventilation was already used, but only provided by Boussignac mask. In 2013 two new ventilators, more sophisticated and more potential, were then purchased by the IMCA department (Falco 202 – Siare®).(13)
The NIV is adopted in the Internal medicine Intensive Care Unit (I.I.C.U) of IMCA, that currently has 8 beds with the possibility of ventilation and careful patient monitoring.
To date, there isn’t any national or international protocol that indicates when to prefer NIV to other treatments. In IMCA department of the Polyclinic Hospital of Modena it was then drawn up a protocol for the use of NIV, intended for patients suffering from respiratory failure with PaO2<70 mmHg and pH <7.35. According to this protocol based on the patient’s initial arterial blood gases (hypoxic hypercapnic or hypoxic hypo-/normocapnic) it can be decided whether to start NIV in CPAP or BiPAP mode (Boussignac or by ventilator), respectively.
NIV in CPAP mode: performed in 1-3 cycles of CPAP (5-12 cmH2O) of 2 hours each with a 1-hour suspension between them. Between one cycle and the other arterial blood gas analysis needs to be checked carefully. If there isn’t any evidence of efficacy in 12-24 hours, the therapeutic strategy needs to be changed.
NIV in BiPAP mode: set IPAP 12-20 cmH2O, changeable according to the current volume (VC) that needs to be reached (VC = 7-10 ml x kg body weight) and EPAP 4-10 cmH2O. Venous blood gas analysis must be checked 2 hours after the start of ventilation and then every 4 hours. The venous blood gas analysis must be kept under control even if there is a good initial arterial blood gas analysis, together with the continuous monitoring of the oxygen saturation of a patient.
BiPAP may also be used for more days with 24-hours cycles and with suspension during meals. Subsequently the number of hours in which the patient undergoes BiPAP is reduced based on the blood gas values.
Aim of the study
The current study has a descriptive purpose and it aims to characterize the application of NIV inside the Intensive care Unit (I.I.C.U) of IMCA department of the Polyclinic Hospital of Modena. In particular, the study is finalized to assess the prevalence and outcomes of this ventilation method and to correlate them with clinical and biochemical parameters of patients treated from January 1st, 2010 to December 31, 2014.
Materials and methods
A retrospective study was performed on patients hospitalized in IMCA department of the Polyclinic Hospital of Modena during the period between January 1st, 2010 and December 31, 2014. Recruited patients were treated, during their hospitalization in IMCA department, with cycles of NIV, according to the department protocol.
The study collected the following data of the selected patients, through the analysis of the medical records: age, sex, date of admission and discharge, number and type of co-diseases, blood tests, arterial blood gas values, transport used to reach the emergency department (ambulance, own transportation), first diagnosis dispatched by the emergency department, vital signs at the entrance, cardiac ejection fraction, oxygen-therapy early (ambulance, emergency department, department), mode and characteristics of NIV with reference to the pathological cause of dispatch (cardiac, respiratory, sepsis, other causes), therapies during hospitalization, medical advices carried out during hospitalization (cardiology, pulmonary, resuscitation), discharge mode and follow-up at December 31, 2014.
The patient records were analysed and summarized using the common descriptive statistics: for continuous variables were used arithmetic average ± standard deviation, while for binary or categorical variables were used absolute frequencies and percentages proportions.
The data were then distributed and analysed by year of hospitalization. To evaluate the differences between the groups (defined by the different year of hospitalization) were used t-test and linear regression test for continuous variables; chisquare test and linear and logistic regression for binary and categorical variables.
For comparison it has been set an alpha of 0.05, considering significant differences at levels below the alpha set. It was considered statistically significant a value of p <0.05.
Results
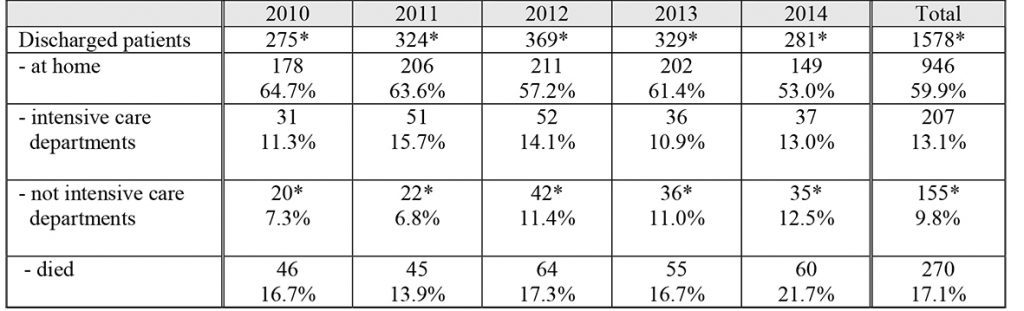
From January 1st, 2010 to December 31, 2014, 1.764 patients were hospitalized in IMCA Intensive Care Unit (I.I.C.U) of the Polyclinic Hospital of Modena. The gender distribution was 60% male and 40% female, with an average age of 75.5 per years. The average length of stay was 7 days. The Tab. 1 shows the data relating to the activity of IMCA Intensive Care Unit (I.I.U.C) of the Polyclinic Hospital of Modena in the period 01/01/2010 – 31/12/2014.
Table 1. Features of the IMCA Intensive care Unit (I.I.C.U) of the Polyclinic Hospital of Modena (data of hospitalized patients, patients treated with NIV and discharged patients in the period 2010-2014 in absolute numbers and percentage of total)
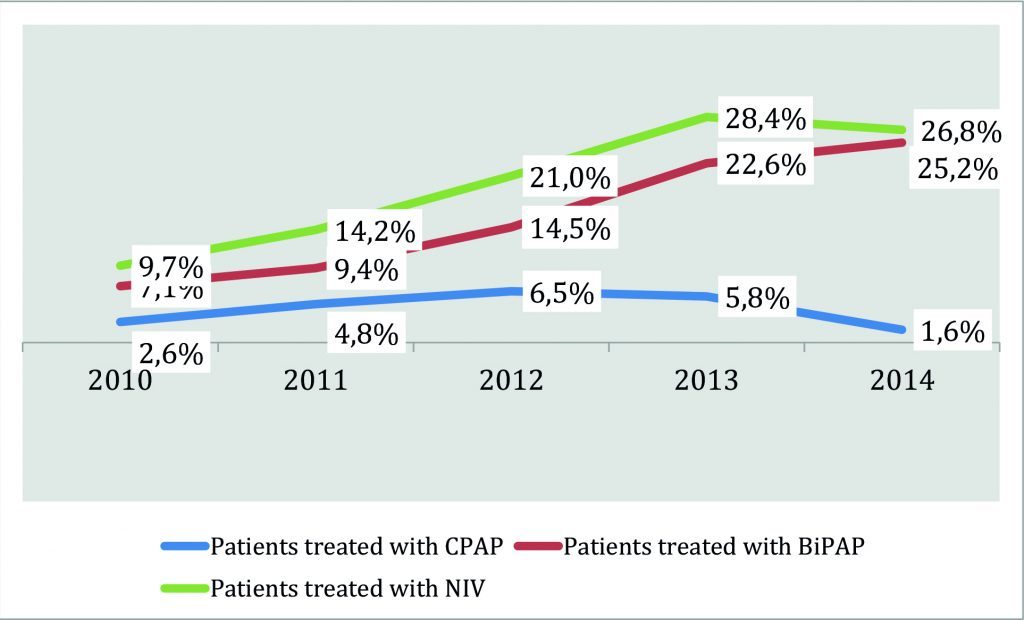
Three hundred and ten patients (310) (over 1.764 of hospitalized patients, the 17.7% of the total), were treated with NIV: looking deeply inside the sample analyzed, 66 patients were treated with CPAP (21,3% of the total 310) and 244 patients were treated with BiPAP (78,7% of the total 310).
As shown in Chart.1, over the years it has been observed a progressive increase, statistically significant, of the percentage of patients receiving NIV (CPAP and BiPAP mode) rising from 9.7% in 2010 to 26.8% in 2014.
Chart 1. Patients undergoing non – invasive mechanical ventilation (CPAP and BiPAP mode) on the total of hospitalized ones in IMCA department of the Polyclinic Hospital of Modena: variation in percentage per year of admission.
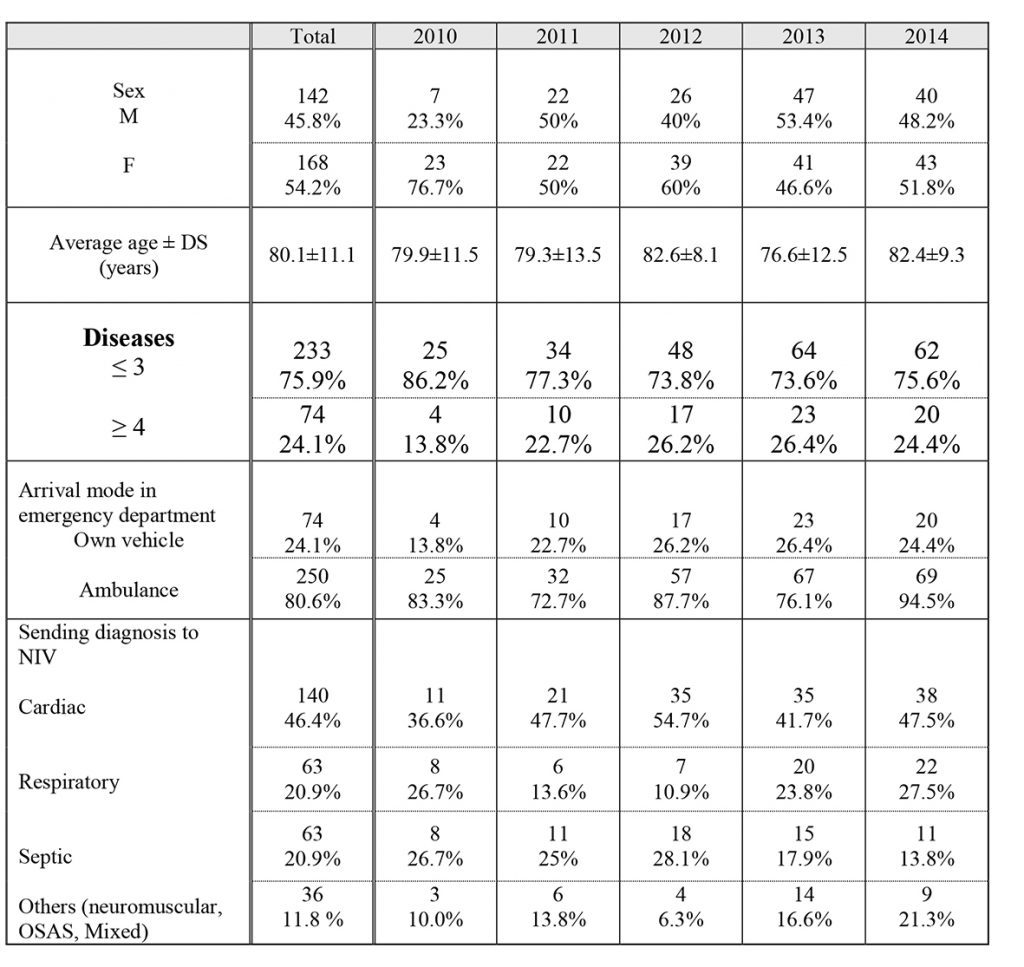
Table 2 shows the general features of the patients undergoing NIV with the arrival mode in the emergency department and the cause that determined the start of ventilation. The larger proportion of patients consists of females (54% versus 46% of males), the average age is around 80 years and patients with multiple diseases, defined as having four or more chronic diseases, representing approximately 25% of the total. The number of patients undergoing NIV who came to the hospital by ambulance remains clearly dominant, with a percentage of 81% over the 5 years of observation.
For what concerns the diagnosis that conducts to NIV, during the years of observation it has been noticed a prevalence, not statistically significant, of the heart cause compared to others. The trend over the years shows a progressive increase in the proportion of patients with respiratory causes in 2012, while for the other two causes such behaviour has not been underlined.
Table 2. General characteristics of the population of patients undergoing NIV in the IMCA Intensive Care Unit (I.I.C.U) in the period 2010-2104: breakdown by year of hospitalization in absolute numbers and percentage of the total.
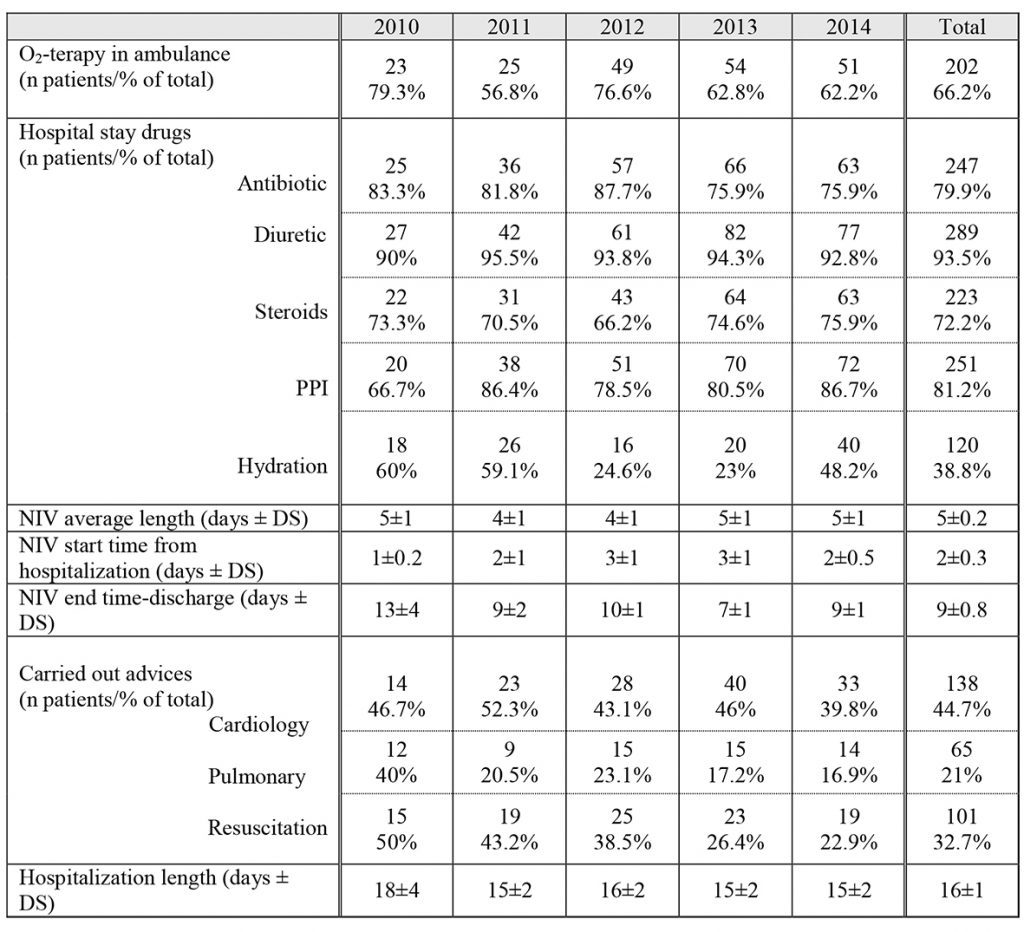
Tab. 3 shows the data related to the treatment of patients undergoing NIV, analyzed by year of hospitalization. The oxygen-therapy is used already in ambulance in the majority of cases (on average in 66% of patients), toward 80% of patients that are dispensed with antibiotic, the 93% is subjected to diuretic therapy, 72% to steroids (predominantly inhalers), and 39% of the patients is subjected to filling fluid challenge of at least 1000 cc/day. Among the non-specific drugs for the treatment of the ARF, more than 80% of patients were undergoing treatment with proton pump inhibitors.
The trend in the adoption of these drugs during the various years of hospitalization, with few not significant variations, was stable without showing significant trends.
Tab. 3 shows also the data related to the beginning of NIV, from 1 to 3 days from the start of hospitalization in each year of study, and the duration of NIV, around 4-5 days. It also gives details about the period of time spent from the end
of NIV and the patient discharge from hospital: with the exception of the first year of the protocol application, where this figure stood at around 13 days, in other years were recorded values of about 10 days.
The average hospitalization length is 16 days, a decrease in the years 2011 to 2014 compared to 2010 (around 15 and 18 days respectively).
Table 3. Therapeutic characteristics of patients undergoing non-invasive ventilation during hospitalization in the IMCA Intensive Care Unit (I.I.C.U): data of the years 2010-2014.
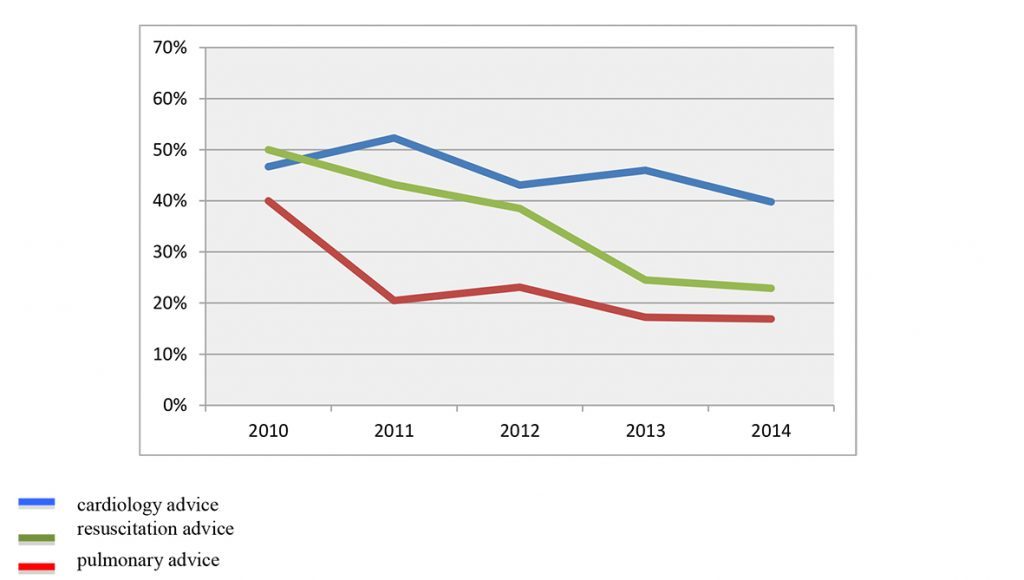
As evidenced by Chart 2, during various years of study, there is a progressive decrease in both pulmonary advices (from 40% in 2010 to 17% in 2014), and resuscitation advices (from 50% in 2010 to 17% of 2014). In both cases it has been observed a linear trend that reaches statistical significance for resuscitation advices. Instead this trend is not clear for cardiology advices that decrease approximately from 50% in 2010 to 40% in 2014, showing although no significant fluctuations over the years.
Chart 2. Percentage of patients undergoing cardiology, pulmonary or resuscitation advices: breakdown by year of admission (the blue line indicates cardiology advice, the red line indicates pulmonary advice and the green line indicates resuscitation advice).
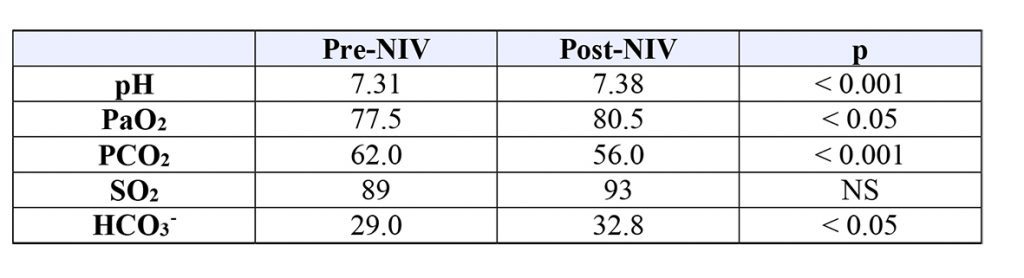
Table 4. Respiratory gas characteristics on arterial blood (pre-NIV values and post-NIV) of the total patients admitted into IMCA Intensive Care Unit (I.I.C.U) for the years 2010-2014.
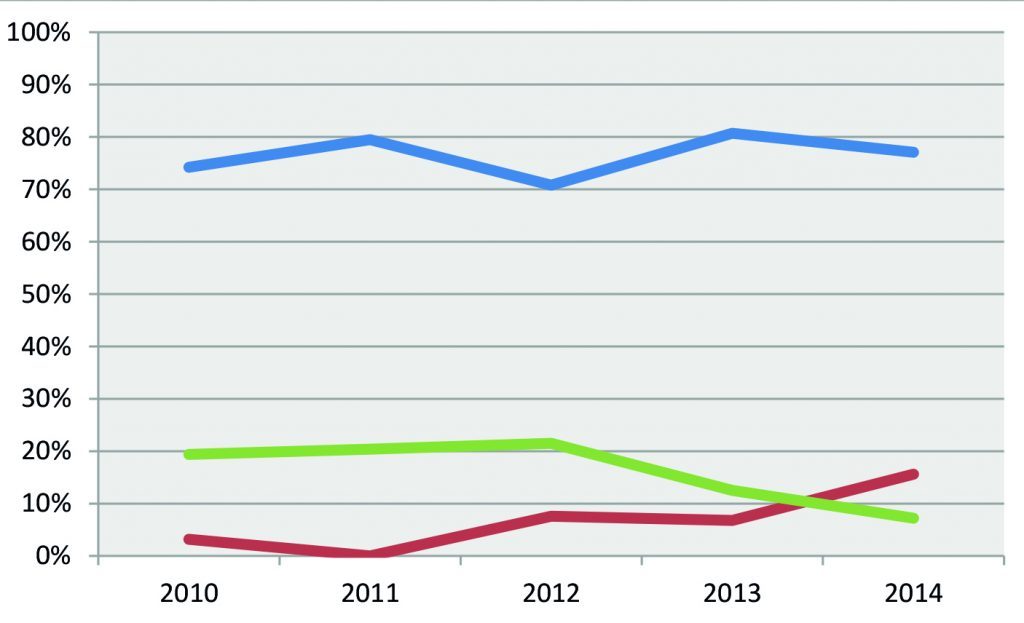
Concerning the data on patients transferred to other departments of the Polyclinic Hospital of Modena, both long-term care and ordinary stay department and intensive ones (Respiratory Intensive Care Unit-RICU and Post-Operative Intensive Care-POIC), it results that on average, 77% of patients haven’t been transferred in any other department. Only the 15% of them were transferred in Intensive Care Unit (Respiratory Intensive Care Unit or Post-Operative Intensive Care) and the 8% were not transferred to another non-intensive department/long-term care. Analyzing each year, as shown in Chart. 3, it appears that the non-transferred patients remained essentially the same, while the proportion of transferred patients to intensive departments decreases from 2012 to 2014, from 22% to 7%, mainly because of the reduction in transfers to Post-Operative Intensive Care (POIC). This trend is associated with a corresponding increase of the number of transferred patients in other non-intensive department.
Chart 3. Percentage of patients not transferred from the IMCA Intensive Care Unit (I.I.C.U)., transferred to another non-intensive department and transferred to Intensive Care Unit (Respiratory Intensive Care Unit or Post-Operative Intensive Care): comparison by year of admission. The blue line indicates non- transferred patients (%), the red line indicates transferred patients to non intensive department (%), the green line indicates transferred patients to Intensive Care Unit (%).
Discussion
This study attempted to evaluate whether the application of a technique, traditionally reserved for Intensive Care Units, could also be effective in an Emergency Medicine department. It was therefore conducted a review of case studies on hospitalized patients in the IMCA I.I.C.U of Polyclinic Hospital of Modena during the period from January 1st 2010, the time of the study start, and December 31, 2014.
According to what has been described above, in IMCA Intensive care Unit (I.I.C.U) the number of ventilated patients with NIV (CPAP or BiPAP mode) on the total of hospitalized, increased progressively over the period. This is due to the progressive increasing skills of the providers involved and to the modernization of available ventilators. Regarding patients undergoing NIV, it must be remembered that these are fragile patients both for the advanced age and for the coexistence of several comorbidity. The average age is around eighty years (80), mostly made up by women, prevalent in this age group. Patients with several diseases are about a quarter of the treated patients and they increase from 2010
to 2014.
Most of the patients come to the hospital by ambulance and for the 40% of cases there is a negative outcome (transfer to intensive care departments or death during hospitalization): similar data were reported in literature. (14),(15)
The main causes leading to treat them with NIV cycles are of cardiology, respiratory and septic nature.
The heart disease is the most represented one since 2010 and it remains like that for all the years of observation: regarding the limited availability of ventilators in cardiology department, patients with heart disease who require NIV are also admitted in IMCA or intensive care unit, justifying such figure recorded.
On the other hand, patients with respiratory diseases undergoing NIV in IMCA department are less than what would be expected and this is due to the fact that most of these patients are hospitalized in the Respiratory Diseases department equipped with an Intensive Respiratory Care Unit. However, the last two years there was an increase also in the percentage of these patients treated in IMCA Intensive Care Unit (I.I.C.U): this could be attributed both to the purchase of the new ventilators in 2013, which allowed the department to treat patients with hypercapnic ARF more effectively, both to the greater confidence acquired by providers.
In these patients, NIV is then started with the specific pharmacological therapy for various patterns of disease. The use of those drugs (diuretics, steroids and antibiotics), mainly administered in patients with cardiac, respiratory and septic diseases, has been studied. During the years there were no significant variations in their use and this is correlated to the substantial stability of the types of patients treated. During the study an high percentage of patients treated with proton pump inhibitors, drugs not related directly to the ARF but among the most prescribed in the general population,(21) has been noticed.
NIV is started on average from 1 to 3 days after admission and continued for 4-5 days. This finding doesn’t change over the years of observation.
It is also interesting to note a decrease of the amount of time between the end of treatment with NIV and the patient’s discharge. This result is probably related to either the effectiveness improvement of the therapeutic approach and to the most experienced operators, together with the modernization of the instrumentation.
Even the reduction of specialist advices requests, particularly pulmonary and resuscitation advices, and the significant decrease of transfers to intensive care department can be evaluated positively, providing further proof that the IMCA health workers training provided by pulmonologists has been effective.
Among the other parameters used to evaluate the effectiveness of NIV, the values of the arterial blood gas of the study population before and after treatment with NIV showed a significant improvement in all parameters.
Concerning the results of treatment with NIV, patients were discharged to home in about 55% of cases, a slightly lower value compared to the total population of hospitalized in IMCA Intensive Care Unit (I.I.C.U).
Regarding this issue, it should be noted that patients ventilated for ARF are on average older (80 years vs. 75.5) and they were suffering from diseases that give a great disability. This should be considered in the interpretation of data related to the percentage of deaths, about 28%, and to the percentage of discharged patients in other healthcare facilities or in residential care homes, about 17%.
Analyzing the trends over the years of patients who died, the trend of patients hospitalized in 2012 becomes evident. In fact it must be remembered that in that year the organization, management and clinical activities within the Polyclinic Hospital of Modena suffered from the effects of the earthquake in May 2012. This calamity caused an increase and a change in the profile of patients admitted in IMCA Intensive Care Unit (I.I.C.U). The analysis of the percentages of the transferred patients in intensive departments during the study period is another indirect efficacy parameter of NIV in U.T.I.I. Area. The trend of transferred patients to Respiratory Intensive Care Unit (RICU) decreases gradually from 2011 to 2014 and also the trend of patients transferred to Post Operative Intensive care (POIC), decreases from 9.7% in 2010 to 1.2% in 2014, with the exception of the year 2012.
Conclusions
Thanks to cooperation with pulmonologists and intensive care specialists, by 2010 it was possible to introduce NIV among the therapeutic modalities provided by the Internal Medicine and Critical Area Intensive Care Unit (I.I.C.U) of the Polyclinic Hospital of Modena. The data analysis has revealed over the years a gradual increase in treated patients and a gradual improvement of indirect outcome parameters, such as transfers to Intensive Care Units and the use of expert advices.
This demonstrates the quality of the training of the department’s health workers and the effectiveness of the modernization of the devices in use.
The ability to treat patients with acute respiratory failure in internal medicine departments might allow to start faster an appropriate treatment and might have a positive impact on the cost/benefit ratio.
References
- Groff P, Cosentini R, Brambilla AM, Causin F, Ferrari G, Giugno B, Maffei A, Mattiazzo M, Piffer F, Purro A. La ventilazione non invasiva: corso NIV SIMEU. Società Italiana di Medicina di Emergenza e Urgenza. Edizione Zero.
- Gregoretti C, Pisani L, Cortegiani A, Ranieri VM. Non-invasive ventilation in critically ill patients. Crit Care Clin 2015; 31: 435-457.
- Struik FM, Lacasse Y, Goldstein RS, Kerstjens HA, Wijkstra PJ. Nocturnal non-invasive positive pressure ventilation in stable COPD: a systematic review and individual patient data meta-analysis. Respir Med 2014; 108:329-337.
- Roussos C, Koutsoukou A. Respiratory failure. Eur Respir J 2003; 47 suppl: 3-14.
- AlYami MA, AlAhmari MD, Alotaibi H, AlRabeeah S, AlBalawi I, Mubasher M. Evaluation of efficacy of noninvasive ventilation in Non-COPD and non-trauma patients with acute hypoxemic respiratory failure: A systematic review and meta-analysis. Ann Thorac Med 2015; 10: 16-24.
- Mas A, Masip J. Non-invasive ventilation in acute respiratory failure. International Journal of COPD 2014; 9: 837-852.
- Keenan SP, Sinuff T, Burns KE, Muscedere J, Kutsogiannis J, Mehta S, Cook DJ, Ayas N, Adhikari NK, Hand L, Scales DC, Pagnotta R, Lazosky L, Rocker G, Dial S, Laupland K, Sanders K, Dodek P; Canadian Critical Care Trials Group/Canadian Critical Care Society Non-invasive Ventilation Guidelines Group. Clinical practice guidelines for the use of non-invasive positive-pressure ventilation and non invasive continuous positive airway pressure in the acute care setting. CMAJ 2011; 183: 195-214.
- Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJV, Ponikowski P, Poole-Wilson PA, Stromberg A, Van Veldhuisen D, Atar D, Hoes AW, Keren A, Mebazaa A, Nieminen M, Priori SG, Swedberg K. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur Heart J 2008; 29: 2388–2442.
- Shirakabe A, Hata N, Yokoyama S, Shinada T, Kobayashi N, Tomita K, Kitamura M, Nozaki A, Tokuyama H, Asai K, Mizuno K. Predicting the success of non invasive positive pressure ventilation in emergency room for patients with acute heart failure. J Cardiol 2011; 57: 107-114.
- Wons AM, Kohler M. Established vascular effects of continuous positive airway pressure therapy in patients with obstructive sleep apnoea-an update. J Thorac Dis 2015; 7: 912-919.
- Fiorino S, Bacchi-Reggiani L, Detotto E, Battilana M, Borghi E, Denitto C, Dickmans C, Facchini B, Moretti R, Parini S, Testi M, Zamboni A, Cuppini A, Pisani L, Nava S. Efficacy of non-invasive mechanical ventilation in the general ward in patients with chronic obstructive pulmonary disease admitted for hypercapnic acute respiratory failure and pH < 7.35: a feasibility pilot study. Intern Med J 2015; 45: 527-537.
- Cabrini L, Landoni G, Oriani A, Plumari VP, Nobile L, Greco M, Pasin L, Beretta L, Zangrillo A. Non-invasive ventilation and survival in acute care settings: a comprehensive systematic review and metaanalysis of randomized controlled trials. Crit Care Med 2015; 43: 880-888.
- Ugurlu AO, Sidhom SS, Khodabandeh A, Ieong M, Mohr C, Lin DY, Buchwald I, Bahhady I, Wengryn J, Maheshwari V, Hil NS. Where is Non-invasive Ventilation Actually Delivered for Acute Respiratory Failure? Lung 2015.
- Khalid I, Sherbini N, Qushmaq I, Mohammad R, Qabajah RN, Nisar A, Khalid TJ, Hamad WJ. Outcomes of patients treated with non-invasive ventilation by a Medical Emergency Team on the wards. Respir Care 2014; 59:186-192.
- Faden HS, Ma CX. Trends in Oral Antibiotic, Proton PUMP Inhibitor, and Histamine 2 Receptor Blocker Prescription Patterns for Children Compared Whith Adults: Implications for Clostridium difficile infection in the Community. Clin Pediatr 2015; 5
- Brugioni L, Gozzi C, Palmieri P. Efficacia della ventilazione non invasiva nel reparto di Medicina Interna Area Critica del Policlinico di Modena. Uno studio retrospettivo osservazionale. Italian Journal of Emergency Medicine 2014; 5.