- Paolo Balzaretti
- Commentaries
Thrombolysis for pulmonary embolism
- 3/2016-Ottobre
- ISSN 2532-1285
What we already know about this topic
Even if its use has been extensively investigated for the last 40 years, thrombolytic therapy for pulmonary embolism still remain a heavily debated intervention in Emergency Medicine. Recommendations from recently published guidelines can be summarized as follow:
- For clinically unstable patients (mainly defined as presenting with shock or BP < 90 mmHg), thrombolytic therapy is suggested if bleeding risk is acceptable (also defined as “not high” or “less than potential benefit”) (ACEP 2011, AHA 2011, ACCP 2016).
- Thrombolysis may be considered for patients with submassive PE (or intermediate risk PE) with signs of clinical (mainly hemodynamic) deterioration after anticoagulation has been started, when bleeding risk is low (AHA 2011, ESC 2014, ACCP 2016). In this case, grade of recommendations is intermediate-low (IIa, IIb, 2C). Submassive (or intermediate risk) PE can be identified in the presence of normal blood pressure associated with either signs of right ventricular dysfunction on an imaging test or elevated markers of myocardial damage or strain (ESC 2014).
- Finally, for low risk PE not showing signs of hemodynamic instability, thrombolysis is not recommended (AHA 2011, ESC 2014, ACCP 2016).
A correct evaluation of bleeding risk appears to be a central issue when considering the use of thrombolysis. Factors associated with higher risk of hemorrhagic complications are increasing age, comorbidities, uncontrolled hypertension; recent stroke or surgery and bleeding diathesis represent contraindications (see reference ACCP 2016 for a complete risk of absolute and relative contraindications).
The Cochrane review ()
Title: Thrombolytic therapy for pulmonary embolism
Authors: Hao Q, Dong BR, Yue J, Wu T, Liu GJ
Bibliographic citation: Cochrane Database Syst Rev 2015; 9: CD004437.
Objective: to assess the effects of thrombolytic therapy in patients with acute pulmonary embolism.
Included studies: randomized controlled trials.
Primary outcome: death from all causes, recurrence of pulmonary emboli, hemorrhagic events.
Secondary outcomes: hemodynamic improvement and thrombolysis (evaluated through clinical signs or angiographic, scintigraphic or echocardiographic, chronic thromboembolic pulmonary hypertension after three, six months and one year follow up.
Number of included studies: 17.
Quality of included studies: all studies presented low or unclear risk of allocation and reporting bias. Four studies were identified as at high risk of overall bias.
Number of patients: 2197
Results:
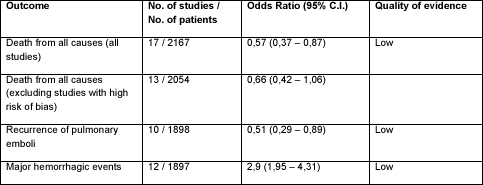
Table 1. Main results. Quality of evidence was determined according to the GRADE system. Major hemorrhagic events were defined as follows: a decreased hemoglobin concentration of > 2 g/dl, retroperitoneal or intracranial bleeding; a transfusion of two or more units of blood, which may or may not lead to discontinuation of anticoagulation treatment. Odds ratios below 1 favor
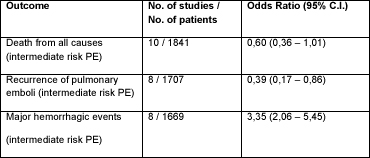
Table 2. Subgroup analysis according to severity of disease. Major hemorrhagic events were defined as follows: a decreased hemoglobin concentration of > 2 g/dl, retroperitoneal or intracranial bleeding; a transfusion of two or more units of blood, which may or may not lead to discontinuation of anticoagulation treatment. Odds ratios below 1 favor thrombolysis.
Thrombolitic therapy was found to decrease pulmonary artery pressure measured by the means of echocardiogram (48 hours after the treatment mean difference was –7,37 mmHg (C.I. 95% -9,20 – -5,53)).
Comment and conclusions
The use of thrombolysis in patients with pulmonary embolism appears to be effective, reducing the risk of death and of recurrence of pulmonary emboli by almost 50%. The effectiveness appears reduced when lower quality studies were excluded. These positive effects were countered by the risk of major bleeding, increased by about 3 times.
These results are broadly consistent with those reported in other systematic reviews (Chatterje et al, Marti et al), published after the completion of the PEITHO trial (Meyer 2014) which, with over a thousand patients enrolled, has a large weight on final estimations of efficacy. Also in the subgroup of patients with intermediate risk pulmonary embolism results were consistent with those of previously published meta-analysis.
Applicability of these results is limited by the width of confidence intervals (with higher bounds indicating only modest benefit) and by the high prevalence of patients with intermediate risk pulmonary embolism; for this reason, risk-benefit balance in high risk patients (poorly represented in the studies included) could be different from the estimation obtained in this meta-analysis.
Overall these results seem to support the approach proposed by international guidelines, reserving thrombolityc treatment to patients who present with low blood pressure or who develop it after the start of anti-coagulation, always taking into account the high risk of adverse events, mainly hemorrhagic ones.
Bibliography
- Fesmire FM, Brown MD, Espinosa JA, et al; American College of Emergency Physicians. Critical Issues in the evaluation and management of adult patients presenting to the Emergency Department with suspected pulmonary embolism. Ann Emerg Med 2011; 57: 628-652.
- Jaff MR, McMurtry MS, Archer SL, et al; American Heart Association. Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension. Circulation 2011; 123; 1788-1830.
- Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE Disease. CHEST Guideline and Expert Panel Report. Chest 2016; 149(2): 315-352.
- Konstantinides SV, Torbicki A, Agnelli G, et al. 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J 2014; 35: 3033-3080.
- Hao Q, Dong BR, Yue J, Wu T, Liu GJ. Thrombolytic therapy for pulmonary embolism. Cochrane Database Syst Rev 2015; 9: CD004437.
- Chatterjee S, Chakraborty A, Weinberg I, et al. Thrombolysis for pulmonary embolism and risk of all-cause mortality, major bleeding, and intracranial hemorrhage. A meta-analysis. JAMA 2014; 311: 2414-2421.
- Marti C, John G, Konstantinides S, Combescure C, sanchez O, Lankeit M, Meyer G, Perrier A. systemic thrombolityc therapy for acute pulmonary embolism: a systematic review and meta-analysis. Eur Heart J 2015; 36: 605-614.
- Meyer G, Vicaut E, Danays T, et al. Fibrinolysis for patients with intermediate-risk pulmonary embolism. New Engl J Med 2014; 370: 1402-1411.