- Tommaso Grandi
- Brief Report and Case Report
Six Cases Of CPR-Induced Consciousness In Witnessed Cardiac Arrest
- 1/2017-Febbraio
- ISSN 2532-1285
Tommaso Grandi(1); Silvia De Carlo(2); Veronica Carosi(2); Alessandra Visentin(2); Nicola Fanton(3); Daniela Baldo(2); Matteo Paganini(2).
1) Emergency Department, Policlinico Casilino, Rome, Italy
2) Emergency Department, University Hospital of Padua, Italy
3) Emergency Department, Ospedale Sant’Antonio, Padua, Italy

Abstract
Chest compressions generate a small but critical amount of cerebral blood flow and occasionally provide sufficient cerebral perfusion pressure to let the patients regain consciousness. CPR-Induced Consciousness (CPR-IC) may be defined as the presence of clinical signs of cerebral perfusion during CPR that are absent when CPR is discontinued. We report six cases of CPR-IC observed in the Emergency Department of the University Hospital of Padova.
Introduction
Current guidelines remark the fundamental role of high quality CPR. Characteristics that affect the quality of chest compression (CCs) are depth, rate, and degree of recoil. CCs interruptions must be minimized to ensure a high percent of total resuscitation time in which compressions are performed, also known as chest compression fraction [1].
CCs generate a small but critical amount of cerebral blood flow and occasionally provide sufficient cerebral perfusion pressure to let the patients regain consciousness; as in previous cases, CPR-IC may be defined as clinical signs of cerebral perfusion during CPR that are absent when CPR is discontinued [2, 3, 4].
In a systematic review made by Olaussen, ten cases of CPR-IC are analyzed: a very variable management is observed, with physical or chemical restraints in six patients and no sedation in the remaining four. The authors also hope for an integration of existing guidelines with identification and management of CPR-IC [5].
Considering the increased attention to prompt initiation of high quality CPR and the diffusion of automatic CPR devices this phenomenon could become more frequent, especially in
cases of bystander witnessed prehospital or intrahospital cardiac arrest. For this reasons the Nebraska Emergency Medical Services has established a sedation protocol for CPR-IC [6].
In a systematic review made by Olaussen, ten cases of CPR-IC are analyzed: a very variable management is observed, with physical or chemical restraints in six patients and no sedation in the remaining four. The authors also hope for an integration of existing guidelines with identification and management of CPR-IC [5].
Considering the increased attention to prompt initiation of high quality CPR and the diffusion of automatic CPR devices this phenomenon could become more frequent, especially in
cases of bystander witnessed prehospital or intrahospital cardiac arrest. For this reasons the Nebraska Emergency Medical Services has established a sedation protocol for CPR-IC [6].
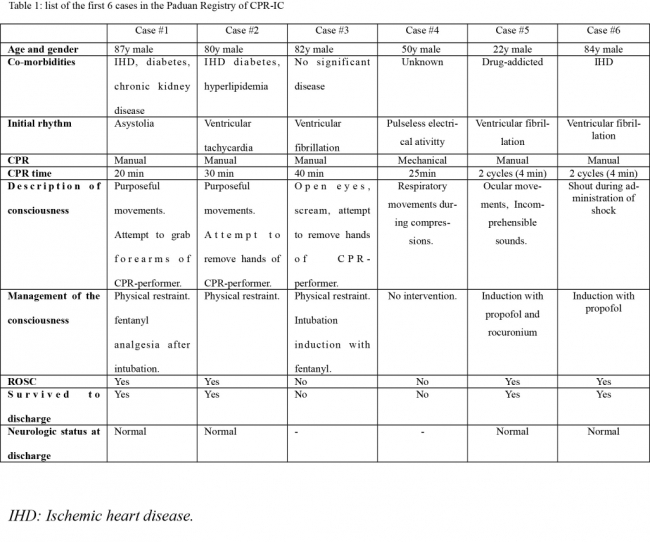
We report six cases of CPR-IC observed in the Emergency Department (ED) of the University Hospital of Padua, from May 2014 to July 2016 (Table 1). Local Ethical Committee
granted an exemption from requiring ethics approval.
granted an exemption from requiring ethics approval.
Discussion
The six cases listed in table 1 were all collected in a unique emergency department in about two years: this suggests that CPR-IC is atypical but not a rare phenomenon. As stated by several authors [2-6], RCP-IC could become more frequent due to diffusion among the population of early and high quality RCP, and of mechanical compression devices.
Consciousness management in these situations is not well known by health-care providers. It could be reasonably considered an index of excellent CPR quality and brain perfusion, although there is no evidence at the moment that could associate it with survival and prognosis. In our experience, four on six patients survived cardiac arrest without neurological impairments after 20 minutes of CPR: further studies are needed to assess these aspects, because it could be considered a reason to prolong resuscitation with the integration, for example, of extra-corporeal circulation (ECMO).
We started manual CCs within 30 seconds from witnessed cardiac arrest. During the first cycles of cardiac arrest algorithm we stopped CPR several times because of misinterpretation with a return of spontaneous circulation (ROSC). After recognizing this situation as CPR-IC we strictly applied ACLS protocol [1], with rhythm check every 2 minutes. For consciousness management we performed physical restraint and/or analgesia (table 1), although it is not clearly defined in current cardiopulmonary resuscitation guidelines [1]; similar management strategies are reported by Olaussenn [5]. The Gordian knot is how to promptly recognize differences between vital signs due to ROSC or to CPR-Induced consciousness. In order to solve it, recommendations for the management of CPR-IC should be implemented, with a special focus on sedation.
Consciousness management in these situations is not well known by health-care providers. It could be reasonably considered an index of excellent CPR quality and brain perfusion, although there is no evidence at the moment that could associate it with survival and prognosis. In our experience, four on six patients survived cardiac arrest without neurological impairments after 20 minutes of CPR: further studies are needed to assess these aspects, because it could be considered a reason to prolong resuscitation with the integration, for example, of extra-corporeal circulation (ECMO).
We started manual CCs within 30 seconds from witnessed cardiac arrest. During the first cycles of cardiac arrest algorithm we stopped CPR several times because of misinterpretation with a return of spontaneous circulation (ROSC). After recognizing this situation as CPR-IC we strictly applied ACLS protocol [1], with rhythm check every 2 minutes. For consciousness management we performed physical restraint and/or analgesia (table 1), although it is not clearly defined in current cardiopulmonary resuscitation guidelines [1]; similar management strategies are reported by Olaussenn [5]. The Gordian knot is how to promptly recognize differences between vital signs due to ROSC or to CPR-Induced consciousness. In order to solve it, recommendations for the management of CPR-IC should be implemented, with a special focus on sedation.
Conclusions
CPR-IC is a phenomenon that implies clinical signs of cerebral perfusion during cardiac arrest and chest compressions. Due to high quality CPR and mechanical compression devices it could become more frequent in the future, so more attention and studies are needed to implement guidelines for a better management.
References
- Kleinman et al. Part 5: Adult Basic Life Support and Cardiopulmonary Resuscitation Quality, 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015;132 Suppl 2:S414–S435.
- Quinn J, Hebert P, Stiell IG. Need for Sedation in a patient undergoing active compressiondecompression cardiopulmonary resuscitation. Acad Emerg Med1994;1:463–7.
- Bihari S, Rajajee V. Prolonged retention of awareness during cardiopulmonary resuscitation for asystolic cardiac arrest. Neurocrit Care 2008;9:382–6.
- Lewinter JR, Carden DL, Nowak RM, et al. CPR-dependent consciousness: evidence for cardiac compression causing forward flow. Ann Emerg Med1989;18:1111–5.
- Olaussen A, Shepherd M, Nehme Z, Smith K, Bernard S, Mitra B. Return of consciousness during ongoing cardiopulmonary resuscitation: A systematic review. Resuscitation 2015Jan;86:44-8
- Rice Dt, Nudell NG, Habrat DA, Smith JE, Ernest EV. CPR induced consciousness: It’s time for sedation protocols for this growing population. Resuscitation. 2016 Jun;103:e15-6.